Message from the Vice Chancellor
Dear Friends,
I am delighted to present you with this 50th Anniversary special edition of our annual report.
UAMS Regional Campuses provide clinical learning experiences for students and family medicine resident physicians to prepare them for practice in Arkansas’ rural and underserved communities. In 2021-2022, our educational programs provided state-of-the-art, interprofessional, team-based training for 157 family medicine residents and 268 UAMS students across the health professions.
With an eye to future generations, our pipeline programs encouraged and supported more than 13,000 high school and college students toward health careers last year.
We collaborated with the UAMS College of Medicine to support the Medical Scholars in Public Health post-baccalaureate program, serving as an educational bridge for Arkansas students who come from socially, economically or geographically disadvantaged backgrounds and have faced challenges in the medical school admissions process.
Our family medicine clinics provide outstanding primary care services to thousands of Arkansans annually. Our faculty, trainees, and staff provide community leadership and outreach through health screenings, rural research, mobile clinics, telehealth services, and many other health- related activities.
Regional Campuses have successfully competed for millions of dollars in federal grants to help support our long-term workforce pipeline programs. These programs span from middle- and high school programs, like CHAMPS and M*A*S*H, through post-graduate primary care training and ultimately rural practice placement.
Finally, I would like to express my gratitude to our affiliated hospitals, community partners, and supporters, as well for the nearly 600 UAMS Regional Campuses team members doing excellent work across our state. We look forward to working with you in the years ahead.
Richard H. Turnage, M.D
Vice Chancellor for Regional Programs
Executive Associate Dean, College of Medicine
Professor of Surgery
Program History
UAMS Regional Campuses, formerly Area Health Education Centers (AHECs), was founded in 1973, through combined efforts of the Governor, the State Legislature, and the University of Arkansas for Medical Sciences (UAMS), as a means to encourage UAMS medical school graduates to remain in Arkansas, and help address the state’s shortage and uneven distribution of primary care physicians. Over time, our mission has expanded to include other disciplines such as pharmacy, nursing, physician assistants and behavioral health professionals.
UAMS Regional Campuses serves as an educational outreach network for UAMS and the principal means to decentralize medical and other health professions education throughout the state. Eight teaching centers in Batesville, Fayetteville/Springdale, Fort Smith, Jonesboro, Pine Bluff, Texarkana, Magnolia, and Helena- West Helena expose future health professionals to underserved communities and provide more varied hands-on experiences than they might receive in a traditional urban, academic
environment. Each center serves a multiple county region
Mission
To improve the health of Arkansans, through community and academic partnerships, by training health professionals and delivering quality patient-centered primary care.
Training Approach & Overview
Quality training experiences in settings away from the academic medical center expose trainees to opportunities in underserved communities, helping encourage rural practice choices. The interprofessional team-based teaching atmosphere enhances the rural professional environment, aids in provider retention, and ultimately strengthens the participating community health care systems.
2021-2022 Trainee Overview
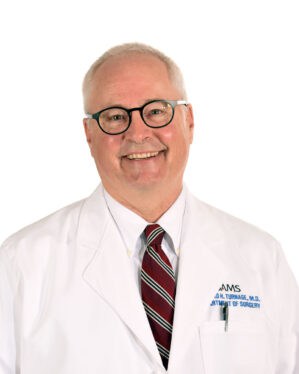
This year, we provided training for:
- 268 health professions students
- 157 medical residents
- 1,212 high school and college students for structured health career programs, and 12,926 in group presentations/events
2021 – 2022 Trainees
Recruiting Students into Health Careers
Before a physician is ready to see patients, their academic journey begins up to 15 years prior. They must be sure to select the required math and science courses starting as early as 9th grade in order to prepare them for future success in medical school. Thus, a long-term pipeline investment is vital. After a pause in face-to-face programming in 2021 and 2022 due to pandemic restrictions, many of our programs were able to return this year.
Student Programs
UAMS Regional Campuses offer high school and college students a variety of programs to explore and advance toward a health career.
High School Students
Day in the Life, MASH, CHAMPS, Hands-on Health Care, ACT prep, Club Scrub, Medical Interpreting, Med Table Talks, and Find Your Future in Healthcare.
College Students
Individual advising sessions, MCAT prep, mock interviews, professional application review, assistance with writing personal statements,
job shadowing, and volunteer/community service.
Regional Recruitment Specialists
Regional recruitment specialists are available in all eight regions of Arkansas. They serve as mentors and academic advisors to connect students with opportunities and resources in their respective regions. Students, parents, teachers, or guidance counselors can find and reach their recruiter below.
Find a RecruiterEmail a Recruiter by Region
M.A.S.H. is Back!
This year, we celebrate 35 years of MASH!

After two years of COVID restrictions, Medical Applications of Science for Health (MASH) and Community Health Applied in Medical Public Service (CHAMPS) returned in Summer 2022. To ease the transition back to in-person programs, we created more flexibility for hosting facilities, offering a choice of one- or two-week MASH programs for 11th and 12th-grade students, and three- to five-day CHAMPS camps for 9th and 10th-grade students, while also continuing a two-day virtual Find Your Futures option.
In 2022, 230 students re-engaged in 20 different camps. In 2023, a total of 27 summer camps resumed statewide, with over 300 participants. Students interact with a wide variety of healthcare professionals, including physicians, nurses, physician assistants, medical/radiologic technologists, respiratory therapists, pharmacists, and dietitians, among others.
Participants learn to identify various disciplines, what they do, how they relate to one another, and how fundamentals of basic science apply to each discipline. Programs offer a variety of topics and hands-on experiences, depending on location, which may include CPR & First Aid training, dissections, suturing, casting, mental/behavioral health, opioid/substance abuse awareness, social media safety, telemedicine, blood typing, tours of local hospitals, provider shadowing, and mock trauma scenarios.
Finally, students learn about available jobs in healthcare and the education and training options in Arkansas, as well as admissions processes and potential scholarships offered through area colleges and universities.
MASH & CHAMPS programs are FREE to participating students, which is made possible thanks to our long-term partners at Arkansas Farm Bureau. To mark MASH’s 35th anniversary, Arkansas Farm Bureau this year established a new Fund for Excellence, pledging $500,000 over the next five years to help guarantee the sustainability of these programs into the future.
Adding Innovation to Education

This new unit joins a growing fleet of mobile classrooms that can reach students in MAS*H and CHAMPS camps in rural communities statewide, and will also be available for other student and professional trainings and community outreach events as needed.
Students will be led through medical scenarios by highly trained simulation technicians, learning and practicing clinical skills, all while connecting these learning experiences directly with local workforce needs.
In partnership with the UAMS Simulation Center, an innovative new Mobile Simulation Classroom will be hitting the road in 2023-24.This mobile unit is equipped with state-of-the-art resources, including simulation manikins, providing learners with hands-on healthcare patient and clinical skills practice in the context of various health career scenarios. Additionally, the unit features an Anatomage 3D virtual dissection table, which offers an unprecedented level of cutting-edge technology, providing extremely accurate and life-like anatomy exploration for a truly interactive and immersive learning experience.
This new venture makes a groundbreaking addition to Arkansas’ healthcare education landscape, marking a significant milestone in the advancement
of healthcare education in the state.
The unit is funded through an Arkansas Simulation Education Training (AR-SET) grant, as a competitive Area Health Education Center (AHEC) supplemental extension under our HRSA AHEC Point of Service Maintenance and Enhancement (POSME) grant.
Rural Student Summit & Field Trip

In Spring 2022, the Student Rural Health Summit and RuralStudent Field trip, were combined to better accommodate the academic calendars of Arkansas’ three medical schools. These annual events were first piloted in 2018 as a core initiative of the Rural Health Association of Arkansas (RHAA). The newly combined event represents a collaboration of UAMS, ARCOM and NYIT, bringing together MD and DO students from all three medical schools in Arkansas.
This year’s event brought together 58 students representing their schools’ rural interest clubs. They convened Thursday at the Winthrop Rockefeller Institute (WRI), situated at the scenic pinnacle of Petit Jean Mountain, to discuss their shared visions of a future in rural practice, to participate in panel discussions with practicing rural providers, and to hear from their schools’ leadership teams. Students rated the experience as fun, enlightening, and impactful.
This was an AMAZING opportunity, and I am so grateful for my decision to attend. I will be reaching out in my third/
Field Trip Participant
fourth years to do a rotation at these clinics so I can further see them in action and what it is like to work there. This
field trip really solidified my stance on going rural.
Clinical Training Excellence
The core mission for Regional Campuses is to encourage more students to pursue a career in primary care, especially Family Medicine. A key focus in recent years has been collaborative efforts of the UAMS Department of Family & Preventive Medicine (DFPM) working with our regional faculty to improve clinical experiences for medical students rotating through our Family Medicine clinics. We recently received confirmation that these efforts are succeeding!
The Association of American Medical Colleges (AAMC) surveys graduating senior medical students regarding their experience in medical school. This survey is used as a quality improvement tool by the Liaison Committee on Medical Education (LCME), the accrediting body for medical schools, as well as the Dean of the College of Medicine.
Of the questions dealing specifically with Family Medicine rotations at UAMS:
- When asking students to “rate the quality of your educational experience in Family Medicine”. This year, 90% of UAMS students rated their educational experience as “good or excellent”, which is the highest score received in the 15 years of this survey.
- When asking students to rate the effectiveness of faculty teaching. This
year, 83% of students agreed or strongly agreed with the statement “faculty provided effective teaching”, which is again the highest score our faculty have received in the past 15 years of this survey.
We are very proud of our faculty and staff that have driven such progress and we are committed to continue providing excellent teaching and clinical experiences for all students.
Clinical Training Excellence – Faculty Spotlight
Leslie Stone, MD, MPH

“I grew up in a small town in Northwest Arkansas and ended up at UCA, where my interests in public health and patient care led me to medical school. In my third-year family medicine clerkship at UAMS the light came on for me. For the first time, I was able to connect with faculty who shared and were supportive of my interests.
After that, I knew I wanted to pursue Family Medicine and ultimately matched to the residency program in Fayetteville. I received excellent training and learned the importance of a patient-centered and broad worldview approach to healthcare.
The Northwest patient population includes many Marshallese and migrant workers, so I learned to consider social determinants that influence a patient’s health, reinforcing my interest in public health.
Working with disadvantaged populations helped build resilience in me, and the strong connections made during residency left me with life-long friends and colleagues that I still draw upon for support. After residency, I worked at a federally qualified health center (FQHC) in Arkansas for 3 years, and then moved to New York to pursue an MPH while working at another FQHC. My training helped prepare me to thrive in diverse and challenging settings.
Now, as DFPM faculty and clerkship director, my goal is to encourage more students to fall in love with Family Medicine like I did. We’ve implemented many improvements in our clerkship. My hope is that when students finish our clerkship, even if they don’t choose Family Medicine, they will understand that primary care is the very foundation of our entire health care system. I try to bring meaningful engagement to the curriculum. Students can’t thrive in isolation. The more engaging and interactive the teacher/learner/ peer relationships are, the better it is for both students and faculty. I like to nurture students’ personal interests by connecting them with mentors and meaningful experiences.
The most effective docs are not just good with patients, but also well versed in population health, social determinants, and how policy impacts the communities they serve.”
Jennifer Casey, MD

“I’m a native of Little Rock and a first-generation college graduate.
In high school, I attended a UAMS summer program called Bridging the Gap, which offered my first glimpse into healthcare. I graduated from the UofA with a Microbiology degree and was accepted to UAMS. The first two years were challenging, but support from peers and faculty made all the difference. I got involved in the Student National Medical Association (SNMA) and was elected president, which helped me further connect with faculty and other medical students.
After graduating medical school, I chose the Family Medicine residency program at UAMS South Central because it allowed me to assist in ALL aspects of medicine, emphasizing prevention. The Pine Bluff residency felt like family. I wasn’t treated like “just a resident,” I was a doctor, a respected member of the healthcare team and community. I was able to grow my medical knowledge under the leadership of physicians with decades of experience, gaining confidence and learning the importance of doctor-patient communication.
I accepted a faculty position in the Pine Bluff program after graduating in 2010. For 4 years as faculty there, I assisted in teaching residents in both inpatient and outpatient settings, as well as medical and nursing students. My career has now come full circle, back at UAMS in Little Rock, as faculty in the Department of Family Medicine (DFPM). I am now helping to influence doctors of the future. I’m excited about the new Honors in Underserved Primary Care program.
As DFPM faculty mentor and advisor for 1st- and 2nd-year medical students, I want them to feel open to approach me with questions.I always tell them, “Anything is possible. You can aspire to do and be whatever you want.”
For me, Family Medicine has provided tremendous personal fulfillment and it is one of the most flexible careers in medicine. The best part of teaching is passing on what I’ve learned in my own journey and cheering these students on. I absolutely love what I do! “
Celebrating 50 Years!
2023 Marks the 50th Anniversary of UAMS Regional Campuses/Arkansas AHEC Program!
The Area Health Education Center (AHEC) concept emerged in 1970, when the Carnegie Commission on Higher Education published a report, “Higher Education and the Nation’s Health: Policies for Medical and Dental Education.” AHECs were to be satellite educational programs developed as extensions of, but at a distance from, major health sciences campuses.
In 1973, the Arkansas Area Health Education Centers (AHEC) program was established by UAMS leadership (Dr. Winston K. Shorey, Dr. James L. Dennis, Dr. Roger B. Bost), Governor Dale Bumpers, and the Arkansas General Assembly with State funding for six regions.
These sites were selected according to their regional locations, as well as their capacity to serve as effective health care training sites, with adequate facilities, varied and qualified healthcare professionals to serve as clinical faculty, and overall community support.
By 2007, two new RURAL regions were added, for a total of 8 regions and AHEC was re-branded as UAMS Regional Programs/Campuses.
Arkansas was one of the first in the nation to undertake AHEC development as a state-supported endeavor, with these objectives:
- To train more primary care physicians, especially family practitioners.
- To retain more graduates of the College of Medicine for practice in Arkansas; and
- To improve geographic distribution of physicians throughout the state.
In 1986, Arkansas received its first federal AHEC grant from the Health Resources & Services Administration (HRSA). Since then, HRSA grants allowed us to expand into comprehensive, fullservice, primary care training centers.
Federal AHEC funds help support long-term workforce pipeline programs, which have encouraged thousands of Arkansas students to pursue health careers. AHECs/Regional Campuses provide interprofessional health professions student education in rural and underserved settings, CME programming, faculty development, and strategic partnership initiatives.
UAMS Regional Campuses/AHEC’s multi-disciplinary faculty teams and resident physicians provide primary care services to 50,000 Arkansans annually, while training an average of 157 Family Medicine residents and 265 health professional students each year. Family Medicine physicians trained by our residency programs currently practice in 67 of Arkansas’ 75 counties.
Over 50 years, Arkansas AHECs have provided training for:
- 1452 Family Physicians
- 6600 Health Professions Students (ie, medical, pharmacy, physician assistant, nursing, social work, and allied health)
- 20,000 High School and College Students in structured health career pipeline programs and academic coaching/advisory roles
- Over 100,000 other middle & high school students were encouraged to consider a health career through large group presentations and events
Timeline of Events
- 1973 The AHEC Program was established, with 6 sites and multi-county regions designated.
- 1974 Three Centers open: Pine Bluff (South Central), Fort Smith (West) and El Dorado (South)
- 1974 – 1976 saw the launching of medical libraries, senior medical student elective rotations, family medicine and internal medicine resident rotations, as well as continuing education programs within each of the initial five sites.
- 1975 Family Medicine (FM) Residencies established in Fort Smith and Fayetteville
- 1975 – 1993 – all original sites established accredited Family Medicine Residency Programs
- 1975 Centers opened in Fayetteville (Northwest) and Jonesboro (Northeast)
- 1976 AHEC Southwest opened in Texarkana
- 1977 FM Residency established in Pine Bluff
- 1980 FM Residencies established in Jonesboro and El Dorado
- 1990 Delta Health Education Training Center (HETC) opens in Helena
- 1993 FM Residency established in Texarkana
- 2001 Delta HETC in Helena expanded to become full AHEC (East)
- 2007 AHEC North Central established in Batesville
- 2013 AHEC South relocated from El Dorado to Magnolia
- 2017 FM Clinic opened in Helena
- 2018 FM Clinic opened in Batesville; Received initial accreditation of their new FM residency program
- 2019 UAMS North Central in Batesville accepted their first cohort of residents
- 2023 Planning begins for a UAMS El Dorado South Campus
Dr. Roger Bost’s Legacy Comes Full Circle
Dr. Gary Berner remembers his granddad, Dr. Roger Bost, as a great story-teller who loved to laugh. “Daju” (as Dr Bost was called by his grandkids) was small in stature, but big in personality.
Dr Bost had a huge influence on Dr Berner and his mom (Virginia Bost Berner). “He was always the one to step up and take care of children who had no other advocate. In the 1950s, he once got word of a critically ill black baby with no place to go for care. Dr Bost brought that baby into the hospital, breaking the rules of caring for non-white patients at that time, and provided lifesaving medications. He was also the first physician in Fort Smith to racially integrate his waiting room.
His helping establish the AHEC program was one of many transformative moves that impacted the entire state. There was so much research and planning that went into it. At that time, the concept of training in rural areas was very progressive and ground-breaking, and he and Gov Bumpers got a lot of pushback. But clearly, he was a visionary and now all Arkansans benefit from the AHEC system.
My mom, a women’s health nurse practitioner providing maternity care for the Arkansas Dept of Health, and my granddad instilled in me the importance of ensuring healthcare access to everyone. When I was in med school, I did a family medicine rotation at AHEC Pine Bluff, where I saw a broad range of practice, did lots of procedures, and experienced really advanced care with community docs.
What I learned from my family and the AHECs led me to practice at Community Clinic, an FQHC model, which serves people from all walks and cultures, regardless of ability to pay. Now I have the privilege of training and instilling that same vision in future providers. Dr. Roger Bost’s legacy is alive and well, in me, my family, and throughout Arkansas.”
Educating Arkansas’ Future Healthcare Providers
Medical Students
UAMS medical students can participate in a Family Medicine Preceptorship and/or a Service Learning Project between their first and second year of medical school, shadowing a family physician or working with our own faculty. This year, 17 students engaged in preceptorships and/or service projects.
In 2021-22, 131 UAMS juniors performed family medicine clerkships at our regional campuses. This mandatory 4-week experience, at a time when medical students are starting to make decisions regarding specialty and practice location, is an important tool for a career in med. and for our res. programs.
This year, 56 senior UAMS medical students completed multiple regional rotations, as did 6 visiting students. Acting Internships are 4-week required rotations focusing on inpatient clinical skills and preparation for residency. The senior year also allows students to design a program of elective rotations to meet personal career goals.
Pharmacy, Physician Assistant, Nursing & Behavioral Health
During 2021-2022, 24 pharmacy students, 25 physician assistant students, 4 nursing students, 1 allied health student, and 1 masters’ level social work intern completed training at one of our campuses. Regional pharmacy and behavioral health faculty enjoy integrated roles in the complex care teams in our family medicine clinics, and in our centers’ scholarly and academic leadership initiatives.
Honors Program in Underserved Primary Care
The new Honors in Underserved Primary Care (HUPC) program enrolls students in their first and second year of medical school, with three core goals:
- expose students medical students by offering a comprehensive, longitudinal extra-curricular experience in rural and urban underserved medicine;
- to sustain medical student interest in practicing primary care in such areas; and
- to retain these medical students in our state once they graduate. To date, 30 students have engaged in the Honors program.
Regional Campuses offer UAMS students opportunities for interprofessional education and hands-on training at our regional locations across the state, including medical, pharmacy, nursing, and behavioral health faculty teams.
Continuity Clinic
First year medical students now also have an early, unique, hands-on opportunity to shadow a community-based primary care physician within an active practice, either in the Greater Little Rock Metro Area (Standard) or in Northwest Arkansas (Accelerated). The minimum requirement is a half-day per week for 4 weeks.
AHEC Scholars
The Area Health Education Center (AHEC) Scholars program is a national initiative engaging students from various health disciplines through clinical, didactic, and community-based activities during the last two years of their professional school curriculum. UAMS Regional Campuses/Arkansas AHEC administers the program and facilitates student connections at the national AHEC level. Medical students in the HUPC Honors program become AHEC Scholars in their 3rd and 4th years. The 2022 AHEC Scholars’ cohort represents 126 medical, physician assistant, pharmacy, and public health students.
UAMS Northwest Launches New Accelerated M.D. Program
The UAMS Northwest campus has launched an accelerated, 3-year M.D. program, which is the first and only such program in the state. The accelerated program is designed to attract medical students who might return to practice in smaller cities and towns, and who want to specialize in primary care fields, like family medicine, internal medicine or pediatrics. This program offers an alternative fast-tracked pathway to train and equip selected medical students early in their career to pursue opportunities in primary care practice.
Our HRSA Medical Student Education grant is providing funding to support this new accelerated M.D. track, as well as to upgrade student education equipment on the main campus and at clinical training sites.
Javier Moreno, Pharmacist
“I grew up in Springdale, Arkansas, and was always interested in science and helping others. In high school I knew I wanted to pursue a career in the medical field so I joined my high school’s medical academy where I would be exposed to medically oriented classes and teachers that could help guide me in the right direction. It was one of my medical academy teachers who told us about MASH. Applying was one of the best decisions I made, because in those two weeks I made many new friends with similar interests as me, I shadowed a variety of healthcare professionals that I otherwise wouldn’t have the opportunity, and I got to learn new skills that I still use to this day as a healthcare professional, such as CPR and blood pressure monitoring!
MASH gave me the confidence to pursue pharmacy. One of the professionals I shadowed was a pharmacist and, after asking her many questions and doing my own research, I no longer felt like becoming a pharmacist was impossible. I attended the UAMS College of Pharmacy, graduating in 2020 after completing my last two years at the UAMS Northwest Regional Campus.
I am now a staff pharmacist in my hometown of Springdale. One of my favorite things about my job is that I am one of the most accessible healthcare professionals in my community. Patients stop by every day asking for my recommendations on what over-the-counter medications are best for them. I have found working as a pharmacist to be a very rewarding experience knowing I am making a difference in my community.”
Training Family Physicians
Family Medicine Residency Programs
Regional Campuses provided training for 157 residents in 2021-2022, including 50 first year, 53 second year, and 54 who completed their three-year residency to become board-eligible in Family Medicine.
UAMS now has 68 first-year Family Medicine residency slots available, including 50 at Regional Campuses, 6 at the Department of Family and Preventive Medicine (DFPM) in Little Rock, and 12 at the new joint DFPM & Baptist Health program in North Little Rock.
UAMS regional residency programs have trained 50 % of all family physicians practicing in rural Arkansas.
Of the 1117 graduates currently active, 885 (79%) are practicing in Arkansas.
Sports Medicine Fellowship
The sports medicine fellowship at UAMS Northwest offers advanced training on diagnosis and treatment of sports- related illness and injury. This one-year fellowship trains two fellows per year, including training with UAMS Health Orthopedics & Sports Medicine, Physicians Specialty Hospital, and in local high schools. The program covers a wide array of sports experiences from collegiate and high school sports to mass participation events.
885 UAMS Regional Campuses-trained physicians now practice in 67 of our 75 counties.
Increasing the number of primary care physicians in Arkansas is urgent, as one-third of those currently practicing are nearing retirement.
Point-of-Care Ultrasound Program
In August 2022, more than two dozen physicians from across the state gathered at the UAMS Department of Family and Preventive Medicine (DFPM) in Little Rock for a two-day training session that served as a first step in a program to expand the use of point-of-care ultrasound.
Point-of-care ultrasound (POCUS) is a tool that helps doctors diagnose patients more efficiently, reducing the need for return visits. Ultrasound devices have the potential to improve diagnosis in rural areas that have less access to specialty care. These physicians are laying the foundation for Arkansas to become a national leader for POCUS in primary care. While well known for its use in obstetrics, ultrasound can also detect gallbladder or pulmonary conditions, guide procedures such as joint injections, and evaluate cardiac function. POCUS devices are now in place at our regional clinics in Batesville, Fayetteville, Fort Smith, Jonesboro, Pine Bluff, Texarkana, and in Little Rock.
Fifteen physicians were selected for a yearlong fellowship through the Global Ultrasound Institute, which led the training. Fellows will receive one-on-one mentorship and training in ultrasound techniques, with a goal of earning credentials so they can train residents at their clinics.
Providing Quality Healthcare for Arkansans in Rural Areas
Clinical Patient Care Our regional family medicine centers provide comprehensive primary care for thousands of Arkansans across the state. Our faculty, residents, and staff are very active in their communities, serving on national, state, and local advisory boards and committees. They provide a vast array of healthcare services, screenings, support groups, and other resources.
Clinic Patient Services 2021-2022
- Patients Served 48,966
- Visits 151,198
Regional Cancer Patient Navigators
In 2022, the UAMS Winthrop P. Rockefeller Cancer Institute implemented a new statewide patient navigation program to help cancer patients across the state access prevention, screening, treatment, and support services. Cancer Patient Navigators are in each of our regional campuses. The program serves all Arkansans regardless of provider, and a physician referral is not required. Cancer patient navigation programs have emerged over the last decade as an e昀昀ective strategy in improving patient access to the full continuum of cancer care. The program is a key piece of the Cancer Institute’s progress toward becoming a National Cancer Institute (NCI) designated cancer center. To connect with a navigator, patients may call 1-855-569-3691 or email COE@uams.edu.

“We know advances in cancer treatment may not reach underserved communities, especially in low socioeconomic areas and among racial and ethnic minorities. Cancer navigation is critical to improve access to cancer prevention and care.”
~ Pearl McElfish, Ph.D., associate director of Community Outreach and Engagement at the Winthrop P. Rockefeller Cancer Institute.
Reaching out to Arkansas Communities
UAMS Regional Campuses’ faculty, staff and trainees engage in many meaningful community service activities across the state throughout the year.

UAMS West Good Samaritan Clinic.
Affiliated Community Hospitals & Partners
Key Partnership Highlights
Arkansas Farm Bureau is our long-term partner making possible M*A*S*H and CHAMPS summer camps across the state. We were thrilled to resume these programs in Summer 2022.
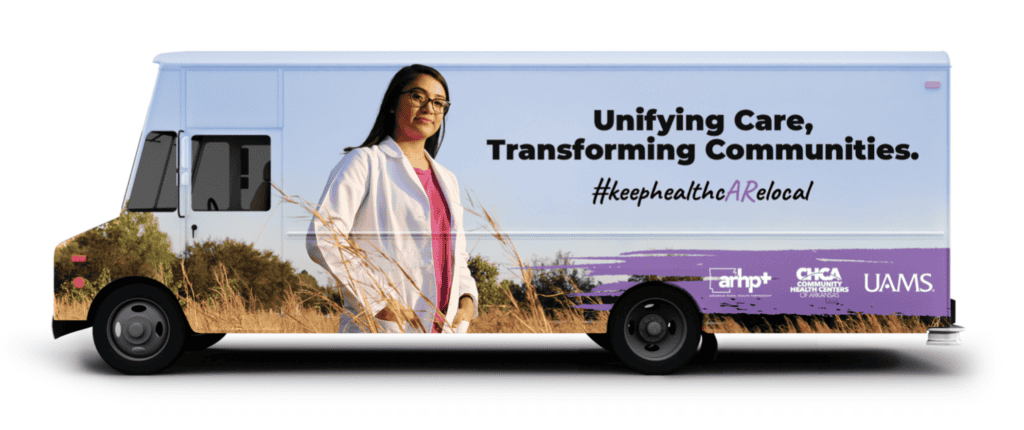
Working with Arkansas Rural Health Partnership (ARHP), more Delta students are being engaged this year through mobile health unit activities and internships at ARHP hospitals.
Through our Community Health Centers partners, we continue to offer clinical and practicum experiences for UAMS students to expose them to federally qualified health center settings.
The mobile unit below is a joint project of UAMS Regional Campuses, College of Medicine, Arkansas Rural Health Partnership, and Community Health Centers of Arkansas, and is funded through the HRSA Medical Student Education grant. Participating students engage in interactive learning about health careers from fellow Arkansans who work in healthcare, and learn about the need for various providers, where they can be trained, how long it will take, and potential earnings. The mobile unit serves schools and communities statewide, including many M*A*S*H camps, and career and health fairs, and is also available for other student and professional trainings and outreach events.
We are grateful for the leadership and commitment of all our faculty, staff, institutional leaders and community partners who are central to the success of our programs. We hold formal affiliation agreements with the hospitals below as host institutions and training facilities. Deep appreciation is extended to these partners, which contribute facilities, funds, and staff to support our programs.
UAMS East
Crittenden Memorial Hospital
Helena Regional Medical Center
Chicot Memorial Hospital
UAMS North Central
White River Medical Center
Baxter Regional Medical Center
Woodlawn Heights Nursing Home
UAMS Northeast
St. Bernards Regional Medical Center
NEA Baptist Memorial Hospital
UAMS Northwest
Washington Regional Medical Center
Northwest Medical Center –Springdale
Arkansas Veterans Home – Fayetteville
Northwest Health Physicians’ Specialty Hospital
Springdale Health and Rehabilitation Center
UAMS South
Magnolia Regional Medical Center
Arkansas Children’s Hospital – Little Rock
South Arkansas Regional Hospital – El Dorado
UAMS South Central
Jefferson Regional
UAMS Southwest
CHRISTUS St. Michael Health System
Wadley Regional Medical Center
UAMS West
Baptist Health Fort Smith
Directory of Regional Campuses
UAMS East
Stephanie Loveless, MPH, Area Director
E-mail: CargileStephanieA@uams.edu
William McClain, Administrative Director
E-mail: CargileStephanieA@uams.edu
Angela Ward, BSN RN AMB-BC, Charge Nurse
1393 Highway 242 South
Helena-West
Helena, AR 72342
Phone: 870-572-2727
UAMS North Central
Faye Turner, Ph.D., Administrative Services Director
E-mail: WFTurner@uams.edu
Jordan Weaver, M.D., Family Medicine Residency Director
E-mail: WFTurner@uams.edu
Kendall Barron, BSN, RN, AMB-BC, Clinical Services Manager
1993 Harrison Street
Batesville, AR 72501
Phone: 870-698-9991
UAMS Northeast
Faye Turner, Ph.D., Administrative Services Director
E-mail: WFTurner@uams.edu
Scott Dickson, M.D., Family Medicine Residency Director
E-mail: SDickson@uams.edu
Bendi Bowers, MSN, RN, Clinical Services Manager
311 East Matthews
Jonesboro, AR 72401
Phone: 870-972-0063
UAMS Northwest
Stephanie Kruger, Administrative Services Director
E-mail: SMKruger@uams.edu
Michael Macechko, M.D., Family Medicine Residency Director
E-mail: MDMacechko@uams.edu
Stacia Dean, BSN, RN, Clinical Services Manager
1125 North College
Fayetteville, AR 72703
Phone: 479-713-8000
UAMS South
Richard Reeves, Administrative Services Director
E-mail: RAReeves@uams.edu
Mimo Lemdja, M.D., Medical Director
E-mail: MLemdja@uams.edu
Jaquetta Hall, BSN, RN, Charge Nurse
1617 North Washington
Magnolia, AR 71753
Phone: 870-234-7676
UAMS South Central
Sheila Huskey, MBA, Administrative Services Director
E-mail: SHuskey@uams.edu
Toni Middleton, M.D., Family Medicine Residency Director
E-mail: TLRasberry2@uams.edu
Tammy Murray, MSN, RN, AMB, BC, Clinical Services Manager
4010 Mulberry Street
Pine Bluff, AR 71603
Phone: 870-541-7611
UAMS Southwest
Phillip ‘Jayson’ Fenters, Assistant Service Line Administrator
E-mail: PJFenters@uams.edu
Matthew Nix, M.D., Family Medicine Residency Director
Sonia Bunyard, BSN, RN, AMB-BC, Clinical Services Manager
300 East 6th (Administration)
3417 U of A Way
Texarkana, AR 71854
Phone: 870-779-6000
UAMS West
Chris Holland, Administrative Services Director
E-mail: CLHolland@uams.edu
Katherine Irish-Clardy, M.D., Family Medicine Residency Director
E-mail: KAIrishclardy@uams.edu
Brenda Morris, RN, Clinical Services Manager
612 South 12th Street
Fort Smith, AR 72901
Phone: 479-785-2431
UAMS Regional Campuses Clinics and Service Line
Shashank Kraleti, MD, Chair DFPM/Director of Service Line
Sandra Meredith-Neve, BScN, RN, CPN, Integrated Medicine, Primary Care, and Population Health Service Lines Senior Nursing Director
Deborah Hutts, MSN, RN, NE-BC, Regional Program Clinics Assistant Nursing Director
Holly Jenkins, MSN, RN, Regional Program Clinics Clinical Specialist
Kathy J. Emans, LCSW, Director of Behavioral Health
Regional Campuses Central Leadership
Richard Turnage, M.D.
Vice Chancellor
Marcia Byers, Ph.D., R.N.
Senior Director
Amber Fluharty
Administrative Services Director
Kwasi Boateng, Ph.D.
Manager of Evaluation
Sarah Eastham
Administrative Services Director
Alex Holladay
Program Education Manager
Robin Howell
Senior Program Manager
Heidi Damron
Education Coordinator
Kendra Koehler
PCTE Grant Manager
Angelica Nunez
Administrative Coordinator/Data
Teresa Leatherman
AR-SET Project Manager
Sheila Williams
Administrative Coordinator