Message from the Vice Chancellor

Amy Wenger, MHSA, vice chancellor
As I reflect on the past year, the COVID- 19 pandemic placed stress on our educational programs, clinical care system, and outreach opportunities. However, at the eight UAMS Regional Campus locations statewide, our care teams of physicians, nurses, care coordinators, behaviorists, and pharmacists during this pandemic put our patients’ care first and are leading the way to improved health care for Arkansans. I am appreciative to our clinical team members and our hospital partners for providing quality clinical care in every region of the state.
As education is a critical core mission across the Regional Campuses’ network of family medicine residency programs and the other pipeline student programs, we met the challenge to safely provide an educational environment, while ensuring trainee and patient care safety. The educational team members showed resilience and perseverance through this past year, while students and residents continued their rotations and received great experiences.
This annual report illustrates some highlights of our educational, clinical, and research activities and programs throughout the state.
Central Program Office
Amy Wenger, MHSA, vice chancellor
Campus Offices
4301 West Markham St (Slot #599 & #599B)
Phone 501-686-5260
Ed South Offices
4021 West 8th St (Slot #599C)
Phone 501-526-4874
Program History
UAMS Regional Campuses, formerly Area Health Education Centers (AHECs), was founded in 1973, through combined efforts of the Governor, the State Legislature, and the University of Arkansas for Medical Sciences (UAMS), as a means to encourage UAMS medical school graduates to remain in Arkansas, and help address the state’s shortage and uneven distribution of primary care physicians. Over time, our mission has expanded to include other disciplines such as pharmacy, nursing, physician assistants and behavioral health professionals.
UAMS Regional Campuses serves as an educational outreach network for UAMS and the principal means to decentralize medical and other health professions education throughout the state. Eight teaching centers in Batesville, Fayetteville/Springdale, Fort Smith, Jonesboro, Pine Bluff, Texarkana, Magnolia, and Helena- West Helena expose future health professionals to underserved communities and provide more varied hands-on experiences than they might receive in a traditional urban, academic
environment. Each center serves a multiple county region
Mission
To improve the health of Arkansans, through community and academic partnerships, by training health professionals and delivering quality patient-centered primary care.
Training Approach & Overview
Quality training experiences in settings away from the academic medical center expose trainees to opportunities in underserved communities, helping encourage rural practice choices. The interprofessional team-based teaching atmosphere enhances the rural professional environment, aids in provider retention, and ultimately strengthens the participating community health care systems.
2020-2021 Trainee Overview
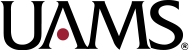
This year, we provided training for:
- 266 health professions students
- 151 family medicine residents (plus 1 fellow)
- 923 high school and college students for structured health career programs
2020-2021 Trainees
Mission Accomplished

Jared Burks is a perfect example of our long-term pipeline to practice mission. We first met Jared as a high school student from the rural northeast Arkansas community of Manila in a summer MASH camp. He remained engaged with our programs throughout college and medical school, and ultimately returned to our regional campus in Jonesboro for residency training. Upon graduation next year, he will return to his hometown of Manila to practice!
What would you say about MASH?
“MASH was great! You see so many options with MASH and you realize there is more to healthcare than just being a doctor or a nurse in a hospital. In college, Yalanda Merrell, UAMS Northeast recruiter offered so much support that helped guide me: Shadowing and volunteering were great exposure, and mock interviews provided a safe practice. I have a stuttering problem when I get nervous, so it was good for me to get that out of my system.”
What advice would you give others who might want to pursue rural primary care?
“Do it, because we need you! It’s a long, tough road, but well worth it. You have to be motivated and have a desire to work with people. Seek out opportunities to see what’s needed in your area that you could provide. Then take full advantage of clerkships and electives in medical school to explore different interests and settings that can help you select a residency and potential practice location. ”
What do you wish someone would have taught you earlier?
“Time management. It’s hard balancing life as a resident and a husband and a dad. But we make it work. And as time goes, it definitely gets better.”
What have been some of the most important aspects of your residency training?
“At UAMS Northeast, we worked with a wide range of specialists, from Cardiology to Dermatology, to Orthopedics, you see a great deal that helps you prepare for what’s ahead in family medicine in a rural community. I’ve learned much more than just patient care. For example, trying to get medications paid for, either because patients have been laid off or because their insurance won’t cover it. I’m learning how to overcome barriers, how to order things a certain way, using the right words, so that’s been really good for me. I want what’s best for my patients, and sometimes that means going the extra mile.”
What experiences have especially helped prepare you for rural practice?
“On a recent Dermatology rotation I was able to do several types of biopsies, that in a bigger city you would just send across the street. But in Manila, I’ll be able to do those same procedures that could have a huge impact on the patient and their overall health.”
Last words:
“It’s been a long journey, Alyssa and I have been through everything together and thank God we are almost back to our hometown of Manila! I’m so thankful to Regional Campuses for being with me and helping to guide and support me at every stage of this journey.”
Health Careers Pipeline
- High School – MASH
The summer of 2009, Jared Burks, a rising senior at Manila High School, was accepted into the Jonesboro MASH program at UAMS. - College – Pre-Med Support
After years of hard work and dedication, in 2015, Jared received his letter of acceptance from UAMS and took his oath as a student in the class of 2019 that fall. - Medical School – MASH Assistant
During the summer between his first and second year, Jared returned home to Northeast Arkansas to be the MASH Assistant for the UAMS Northeast Campus in Jonesboro. - Residency – Back Home
Match Day 2019 for UAMS was held March 15 where Jared announced he was doing his residency in Family Practice medicine at UAMS Northeast in Jonesboro. - Practicing Physicial – Hometown/rural area
Jared is a great example of what the pipeline was intended to do through our Regional Campuses. From MASH to Match, Jared has been plugged in and using all the support that UAMS has offered. After residency, Jared plans to return to his hometown of Manila to practice Family Medicine.
Recruiting Students into Health Careers
Before a physician is ready to see patients, their academic journey begins up to 15 years prior. They must be sure
to select the required math and science courses starting as early as 9th grade in order to prepare them for future success in medical school. Thus a long-term pipeline investment is vital.
In a typical year, UAMS Regional Campuses offer high school and college students a variety of exposure and enrichment programs to explore and advance toward a health career, including:
High School students – A Day in the Life, MASH, CHAMPS, Hands-on Health Care, ACT prep,
STEM enrichment.
College Students – MCAT prep, mock interviews, resume/personal statement assistance, professional application review, and job shadowing/volunteer hours.
In 2020-2021, many in-person programs could not be offered due to COVID-19 pandemic restrictions, but more than 923 high school and college students were still engaged through these and other new programs launched this year, such as:
- Find Your Future in Healthcare is a virtual 3-day health careers exposure/enrichment initiative for high school students created for summer 2021, in lieu of in-person MASH. Two sessions were held June and July.
- This Can be You is a 2-week camp to introduce underrepresented minority high school students to medical career pathways through the state’s HBCUs. This collaboration between University of Arkansas at Pine Bluff (UAPB) Health Professions Prep and UAMS HBCU MedTrack (see next section), took place at UAPB in June-July.
- Arkansas Rural Health Partnership (ARHP) Academy recruited 40 south Arkansas students to work 100 hours each at ten ARHP member hospitals. Participants rotated through all hospital departments. These internship experiences ranged from administration to observing surgeries. Interns attended training sessions on mental health, first aid, and opioids, while also hearing insights from a rural medical student.
- MD Mentors has connected over 120 UAMS medical students with pre-med college students to date, offering sessions on navigating the medical school application process as well as tips and advice on handling medical school.
- Club Scrub at UAMS South Central is a program that has been offered since 2016, in partnership with the Ivy Center for Education in Pine Bluff. This program is designed to introduce students to various career opportunities available in health care with an emphasis on rural and underrepresented minority students and communities. Club Scrub is a seven-month class with objectives to educate participating students regarding the many available careers in healthcare, how to research the specific educational requirements for selected careers, and to provide hands-on experiential opportunities with healthcare providers in the region. The culminating activity is a ceremony where each student receives his or her first white coat, which is a physical reminder that their goal is attainable with support from their community.
Increasing Diversity in Arkansas’ Healthcare Workforce
- The HBCU MedTrack was created in 2020 to guide and support students from Arkansas’ Historically Black Colleges and Universities (HBCUs) and increase their successful matriculation into UAMS colleges. The MedTrack is a partnership between UAMS, University of Arkansas at Pine Bluff and Philander Smith College. HBCU MedTrack students participate in grant-funded Serving Underrepresented Populations through Engagement and Research (SUPER) projects and Medical College Admissions Test (MCAT) prep courses, and a continuum of programs, experiences, and mentoring to guide and support them as they navigate their health professional journey.
- SUPER introduces students to community-based research and health disparities, teaching them the process of conducting research with the guidance of mentors at their home institution and at UAMS.
- An Anesthesia Tech Program was also created to provide students with training and employment as UAMS Anesthesia Techs, while gaining clinical skills and preparing for MCAT and professional applications.
- In May, 15 students were welcomed into the inaugural class of a new UAMS post-baccalaureate pre-med program called Medical Scholars in Public Health. Six of these 15 students came through the HBCU MedTrack! They are pictured below with MedTrack director and mentor, Ms. Renisha Ward.
The post-bacc program is intended to serve as an educational bridge to a master’s degree in public health and/or a medical degree for Arkansas residents who come from socially, economically or geographically disadvantaged backgrounds and who have faced challenges in the medical school admissions process. All of these programs are part of UAMS’ and Regional Campuses’ multi-faceted approach to increase the number of underrepresented minorities, rural and disadvantaged students entering the state’s healthcare workforce. All programs are supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $7 million with 10% financed with non-governmental sources, managed by UAMS Regional Campuses.

Xavius Hymes
What influenced your decision to go to medical school?
“Having sickle cell anemia played a huge role in my decision to go to medical school. My own caring team of physicians and nurses also sparked my interest in the medical field because every one of them have exemplified what it means to have courage, strength, and resilience.”
What’s your best memory of HBCU MedTrack?
“Being a part of the HBCU MedTrack has meant always having an understanding team of peers and advisors around to help point me in the right direction. I strongly recommend joining this program!”
What has surprised you most about working with HBCU MedTrack?
“I’ve realized that many people have similar struggles when it comes to pursuing a career in Medicine. I also learned that you definitely get out of I what you put in. The MCAT was a significant challenge for me and the MedTrack helped me to understand and improve my skills on how to score competitively. Having just been accepted into the new UAMS Post Baccalaureate program, I’m forever grateful for all the guidance and support!”
Maria Meneses Ramos
What influenced your decision to go to medical school?
“It was a culmination of growing up as a first-generation immigrant. I had to interpret for my family because there weren’t any interpreters available at the clinics they attended. Being immersed in this environment early on exposed me to health care, and I realized that I could make a difference in the lives of patients. It became even more fascinating when I was able to apply the lessons I learned in class to actual cases and people!”
What’s your best memory of the Anesthesia Tech program?
“Getting thrown into the OR with my cohort! Although it was daunting in the beginning because we were in the midst of a pandemic, UAMS provided us the tools, training, and skills to overcome. It was such an exciting experience to not only see procedures, but also be assisting in the care of patients, while learning at the same time.”
Please share one of your best experiences to date.
“The best thing to ever happen to me is going through the Anesthesia Tech program. Being in such a position and environment has been so encouraging, and has given me confidence and reaffirmation to pursue my dreams. More than anything, I am extremely grateful for the residents, attendings, CRNAs, nurses, and scrub techs who have been supportive of me while at UAMS. They’ve all given me advice, encouragement, tips, and tricks, which will stay with me on my journey to medical school and beyond.”
What do you wish other people knew about HBCU MedTrack?
“There is nothing like it. This program is versatile, helpful, and opens doors to many opportunities. It can equip you with skills, resources and tools to perform well academically, and also help you make connections and prepare you with life and professional skills needed to succeed and become a well-rounded individual. Ms. Ward works so hard for her students and can connect anyone to the right resources to achieve their dreams.”
Educating Arkansas’ Future Healthcare Providers
Medical Students
UAMS medical students can participate in a Family Medicine Preceptorship program and/or a Service Learning Project between their first and second year of medical school, shadowing a family physician and/or working with one of our own faculty. This year, 12 students completed 10 projects.
In 2020-21, 146 UAMS juniors performed family medicine clerkships at our regional campuses. This mandatory experience, at a time when medical students are beginning to make decisions regarding specialty and practice location, is the most effective recruitment tool to date for our residency programs.
This year, 32 senior UAMS medical students also completed regional rotations, as did 10 visiting students. Acting Internships are 4-week required rotations focusing on inpatient clinical skills and preparation for residency. The senior year also allows students to design a program of elective rotations to meet personal career goals. Pharmacy, Physician Assistant, Nursing and Behavioral Health
Pharmacy, Physician Assistant, Nursing and Behavioral Health
During 2020-2021, 39 pharmacy students, 21 physician assistant students, 3 nursing students and 3 masters’ level social work interns completed training at one of our centers. Regional clinical pharmacists and behavioral health faculty enjoy an integral role in the complex care committees in their respective family medicine clinics, and in their centers’ scholarly activities and academic leadership initiatives.
New Honors Program in Rural & Urban Underserved Primary Care
New Honors Program in Rural & Urban Underserved Primary Care
A new Honors Program in Rural & Urban Underserved Primary Care was launched this year, with three core goals: 1) To train medical students by offering a comprehensive, longitudinal extra-curricular experience in rural and urban underserved medicine; 2) to sustain medical student interest in practicing primary care in such areas; and 3) to retain these medical students in our state once they graduate. Regional Campuses
New Community Health Center Rotations For non-traditional medical student Paula McClain, federally qualified Community Health Centers (CHCs) opened up a whole new world, and even led to her rethinking her career plans. McClain was one of the first of six junior UAMS students to participate in a new multisite CHC rotation offered for the first time this year. McClain admitted she had “no clue” about CHCs before taking part in the program, and found it a very rewarding and worthwhile experience.
New Community Health Center Rotations
For non-traditional medical student Paula McClain, federally qualified Community Health Centers (CHCs) opened up a whole new world, and even led to her rethinking her career plans. McClain was one of the first of six junior UAMS students to participate in a new multisite CHC rotation offered for the first time this year. McClain admitted she had “no clue” about CHCs before taking part in the program, and found it a very rewarding and worthwhile experience.
It made me consider for the first time not going into surgery. It gave me much greater appreciation for being out in a rural clinic. You learn how much health education is really at the heart of good health care.
Paula McClain
Erica Olson, Medical Student

“I am from Gassville, Arkansas, born and raised. I graduated from Cotter High School with 40 other students. Coming from a small town, I considered universities from the West to the East coast. However, I landed back in my home state, at the University of Arkansas at Little Rock, with a full ride scholarship. I got involved with the pre-professional health committee, and then connected with UAMS Regional Campuses.
My desire to go to medical school and become a family physician have always been intertwined. While I always enjoyed science and academic challenges, I found my greatest passion to be helping others, which I knew would guide me to my future career. Family medicine embodies the paradigm of helping others and establishing and maintaining life-long relationships.
I’ve been actively involved in the Family Medicine Interest Group leadership since starting medical school. This allowed me to learn about summer opportunities Regional Campuses offers in primary care settings. Although COVID disrupted many plans, I’ve been able to get involved with MD Mentors and completed a service-learning project. This allowed me to work with top-notch family medicine faculty at UAMS, who are nothing short of inspirational. Dr. Leslie Stone and his team were so impactful, I’ve planned my family medicine clerkship to continue under their fantastic leadership.”
Training Family Physicians
Family Medicine Residency Programs
Regional Campuses provided training for 151 FM residents this year, including 53 first-year, 52 second-year, and 46 who completed their three-year residency to become board-eligible in Family Medicine. Of these, 61% (28/46) remained in Arkansas to practice, 37% (17/46) remained in their training region, and 22% (10/46) chose a rural county in Arkansas.
UAMS now has 68 first-year Family Medicine residency slots available, including 50 at Regional Campuses, six at the Department of Family and Preventive Medicine (DFPM) in Little Rock, and 12 at the joint DFPM & Baptist Health program in North Little Rock.
UAMS regional residency programs have trained 50% of all family physicians practicing in rural Arkansas.
Of UAMS Regional Campuses’ Family Medicine Residency Graduates
- 61% (868/1425) remained in Arkansas.
- 30% (434/1425) remained in their training region;
- 23% (326/1425) practice in Rural* areas.
*Rural: Defined at hrsa.gov/rural-health/about-us/definition/index.html
868 UAMS Regional Campuses-trained physicians now practice in 68 of our 75 counties. Increasing the number of primary care physicians in Arkansas is urgent, as one-third of those currently practicing are nearing retirement.
Expansion of Rural Family Medicine Residency Training Programs
UAMS is committed to growing graduate medical education throughout the state. By doing this, we increase recruitment and retention of physicians who understand and are equipped to care for the specific needs of people in rural communities.
The vast majority (80%) of physicians who complete both medical school and residency through UAMS choose to stay in Arkansas to practice.* UAMS Regional Campuses received two grants in September from the Health Resources & Services Administration (HRSA) to support expansion of rural residency training opportunities in Arkansas. A Primary Care Training & Enhancement (PCTE) grant will help enhance and standardize residency curriculum across our network, and strengthen UAMS infrastructure to roll out additional programs in future years.
UAMS Northwest received a HRSA Rural Residency Planning & Development (RRPD) grant that will support development of a family medicine rural training track (RTT), culminating in four additional graduates per year. The RTT will be connected to the long-standing UAMS Northwest family medicine residency. RTT residents will complete their first post-graduate year (PGY1) of residency at Washington Regional Medical Center.
(WRMC) in Fayetteville, and then spend PGY2 & PGY3 mostly in rural facilities, including Mercy-Berryville Hospital and WRMC and Mercy-affiliated rural clinics. The first group of RTT residents will join the program in July 2023. Ronald Brimberry, M.D., a UAMS graduate and core faculty at UAMS NW for more than 20 years will serve as program director.
UAMS Regional Campuses will continue to assess, plan, and pursue other RTTs across the state.
*Source: 2019 Association of American Medical Colleges, Arkansas Physician Workforce Profile.
Learn more about our residency programs.
New Faculty Spotlight – Sasha Jennings, M.D.

Dr. Sasha Jennings completed her residency June 30, 2021 and will return as faculty at UAMS South in Magnolia on July 17th.
Why did you choose to become a physician?
“I am from a rural community in northeast Georgia and I’ve wanted to be a doctor since I was five. Imagine me taking care of my Raggedy Ann doll! I’ve always wanted to help everyone, so I guess you can say it was in my nature.”
Why did you choose family medicine?
“I chose family medicine after completing my core rotations in medical school because I wanted to take care of patients from birth to death. I love the full scope of family medicine and being a gate keeper for my patients.”
What made you choose residency in Magnolia?
“My heart has always belonged in the country and Magnolia is a rural program. I grew up seeing healthcare gaps that existed in rural communities and wanted to help close those gaps by bringing updated medicine to such areas.”
What do you like about practicing in a rural area?
“I honestly love the fact that in a rural community you all have to depend on and trust one other for the community to thrive. The community respects you wherever you are. I love the lack of traffic and being able to get to work in 5 minutes or less. I love not breathing in smog!”
Why did you choose to stay on as faculty in Magnolia?
“I love this community! Magnolia has amazing small town charm
with easy access to larger cities. The people are wonderful and
it’s a place you can visualize raising your family in.
New Faculty Spotlight, Chase Helm, M.D.

“UAMS Southwest has a great reputation for training well-rounded family physicians who are able to function competently in a variety of settings. My family and I love the area, and I have valued being able to work with and learn from some of the most influential physicians. I look forward to continuing to give back to my home state as I pursue my career as a family physician in my hometown of Magnolia, AR. UAMS Southwest was a major part of my medical journey and I couldn’t be more grateful for the enrichment it has brought to my life.”
Providing Quality Healthcare for Arkansans in Rural Areas

Clinical Patient Care
Our regional family medicine centers provide comprehensive primary care for thousands of Arkansans across the state. Our faculty, residents, and staff are very active in their communities, serving on national, state, and local advisory boards and committees. They provide a vast array of health care services, screenings, support groups, and other resources.
Clinic Patient Services 2020-2021 UAMS West nursing staff
- Patients Served 49,391
- Visits 139,354
Diabetes Expansion
As part of UAMS Vision 2029, our goal is to lead Arkansas to be the healthiest state in the region through its synergies of education, clinical care, research, and purposeful leadership.
Aiming towards this goal, Dr. Joseph Henske, director of the diabetes program for the UAMS Division of Endocrinology, Diabetes, and Metabolism, is teaming up with UAMS Regional Campuses on a Diabetes expansion project. This project will allow core diabetes care services such as consultation for implementation of continuous glucose monitoring and advanced insulin pump systems to be offered more broadly at various regional centers throughout the state. The recent implementation of the EPIC EMR (electronic medical record) at the regional centers brings the clinics on one unified platform, which will aide in enhanced care and management of the individuals living with diabetes throughout Arkansas.
Starting July 2021, Marissa Boggs, an Advanced Practice Registered Nurse within the UAMS division of Endocrinology, will begin offering Diabetes telemedicine services to patients at the Family Medical Center in Helena.
“I requested a telemedicine visit due to Covid exposure. I expected to have to wait several days to be seen, but was surprised to be scheduled
UAMS Southwest patient
a virtual visit just an hour later. Everyone was very courteous and professional. The staff made the entire process quick and seamless, and my prescription refills were sent immediately to my pharmacy. This facility is very thorough and efficient and I highly recommend them.”
Regional Libraries & Other Resources
The UAMS Library coordinates with Regional Campuses to offer medical library resources for area healthcare professionals, students and other trainees in their respective regions. In collaboration with the UAMS Institute for Digital Health & Innovation (IDHI), providers and faculty across the state can easily access a broad range of continuing professional education and lifelong learning resources. See LearnOnDemand.org.
School-Based Health Clinic for Southwest Arkansas
UAMS Southwest has partnered with Fouke School District in Miller County to offer medical care in the Fouke Health and Wellness Center. The Fouke School District was awarded a $500,000 grant from the Arkansas Department of Education to establish a school-based clinic in the medically underserved
rea. UAMS Southwest physicians will see both pediatric and adult patients at the site, providing well child visits, acute care services, sports physicals and Medicare wellness visits.
UAMS Faculty and staff providing care at the center hope to improve health outcomes for Fouke School District’s students, as well as community members. School-based health clinics have been shown to reduce emergency room visits, hospitalizations, Medicaid expenditures, student absenteeism, and school discipline referrals. In addition to providing timely and excellent care, this new clinical outreach setting will expose UAMS Southwest family medicine residents to the unique challenges of an underserved rural community and to a school-based healthcare model, while also extending health careers enrichment programs to Fouke students.
Satellite Transplant Clinics
As of this year, three regional campuses now serve as satellite transplant clinics for UAMS Health’s kidney and liver transplant patients, providing easily accessible follow-up care at UAMS Southwest (Texarkana), Northeast (Jonesboro), and Northwest (Fayetteville) regions. The clinics in Jonesboro and Texarkana joined a satellite clinic that has been operating in Fayetteville since early 2019.
Due to the incredible work of the regional campuses, we have been able to better care for patients in their home communities.
Lyle Burdine, MD, PhD, surgical director for the UAMS solid organ transplant program
In addition to transplant care, the clinics provide dialysis access evaluation; liver, pancreatic and cancer evaluation and care; management of disorders of the bile ducts; and care for liver failure and liver dysfunction.
I am excited about the UAMS satellite transplant center in Jonesboro because it provides greater accessibility to patients who live in Northeast Arkansas, and will promote stronger relationships and collaborations between UAMS and the health care providers in this region.
Scott Dickson, MD, director of the Northeast Regional Campus
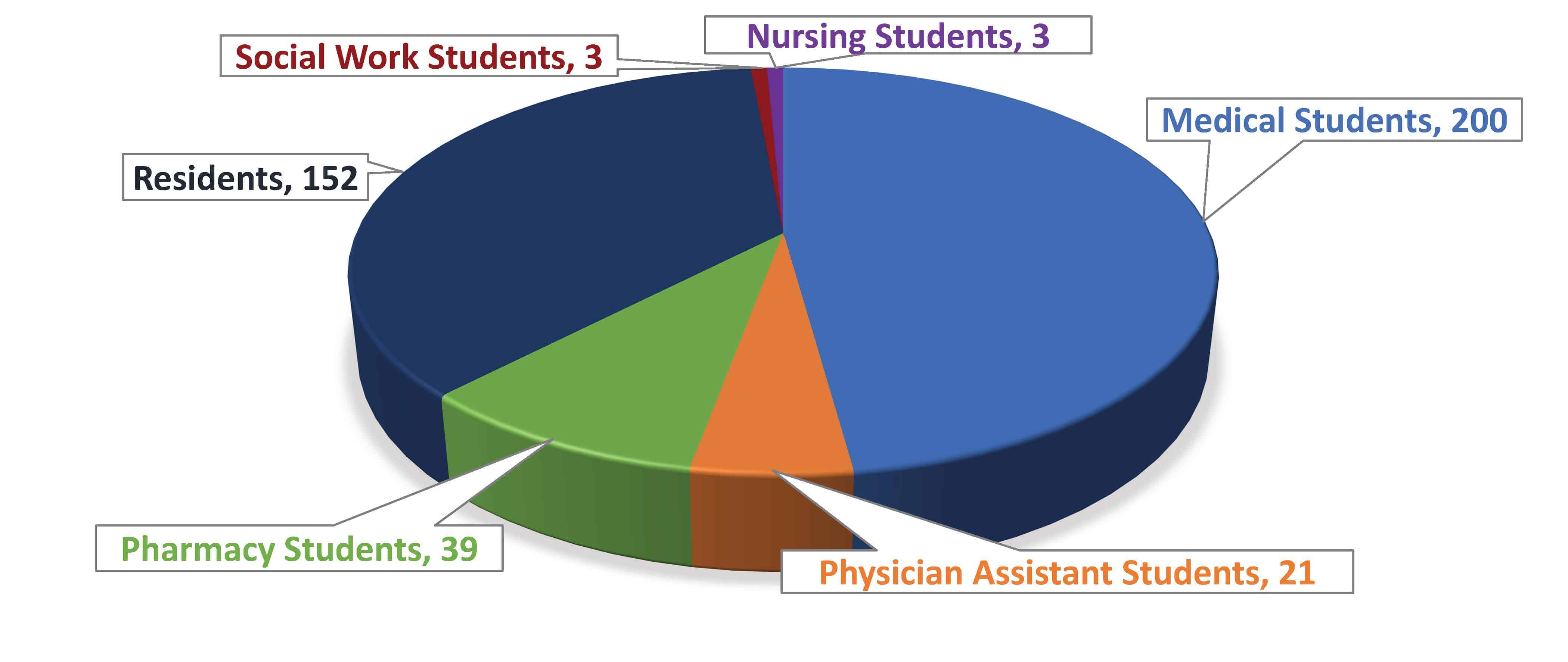
Regional Clinics are ‘EPIC’ – One Patient, One Medical Record, One UAMS Health System
The Regional Campus clinics began their EPIC journey in late 2019 when they began the transition from Centricity to the EPIC Electronic Medical Record (EMR). When completed in 2020, this met Strategic Objective 7 in
the UAMS Health Vision 2029 Strategic Plan: to “Build technology infrastructure to support UAMS’ strategy” with the goal to have all UAMS patients on a single EMR system by 2025.
This will improve continuity and quality of care by having
Dr. Cam Patterson, Chancellor UAMS
appropriate clinical and historical documentation for patients’
records in one system.
Implementing a single EMR has improved the quality of care for patients statewide, whether treated at the main UAMS campus or at one of the regional Family Medicine Centers (FMCs). UAMS inpatient records are immediately available for regional FMC physicians and nurses, and UAMS main-campus staff can access the patient’s regional clinic notes, x-rays, and lab results. This sharing of information not only improves patient care but further promotes a safer patient care environment. Patients comment that having their PCPs and any specialty providers able to view all records improves the thoroughness of their appointment. Patients also like the accessibility to their clinic visit documentation, medication lists, lab results, and upcoming medical appointments through the My Chart portal. One patient, one medical record, is technology at its best.
Tobacco Cessation Services for Regional Patients
Providing tobacco cessation help to regional patients got easier this year. The Magnolia Clinic was first to adopt the new Tobacco Protocol with a January 2021 launch. During the pilot phase, patient referrals were sent to the UAMS
Campus Certified Tobacco Treatment Specialists (CTTS) for management. By July, more than 80 referrals had been made for tobacco cessation consultations. New referrals will soon transition back to regional tobacco treatment specialists to begin providing the cessation services.
While the Magnolia launch was underway, arrangements were made for the MD Anderson Tobacco Treatment Specialist Certification training course, and six Regional Campus staff from Helena, Fort Smith and Texarkana completed the course. The providers in those clinics are now referring patients for in-clinic or phone tobacco cessation consultations.
Roll out of the Tobacco Cessation Protocol and EPIC Smoking Cessation Smart Set Workflow will move forward for the remaining Regional Campuses in the near future.
Reaching out to Arkansas Communities

Team UAMS quickly pivoted, prioritizing COVID-19 vaccinations over testing as the 2020 pandemic shifted gears. When Arkansas opened vaccine eligibility to those over 75 years of age, the Integrated Medicine Services Line team led by Dr. Michelle Krause and Sandra Meredith-Neve, RN, BSNc, CPN directed efforts to provide community vaccine clinics and mobile visits to underserved and rural areas of the state. Regional Campuses have been instrumental in this important effort, developing these programs tailored to fit their individual population health needs and touching almost every county in Arkansas. Over 70,000 doses of COVID-19 vaccinations have been provided through UAMS efforts to date.
The Rural Research Network is innovative, collaborative
Michael J. Birrer, MD, PhD, Director and Vice Chancellor, Winthrop P. Rockefeller Cancer Institute
and practical, enhancing the utilization of an existing resource such as UAMS Regional Campuses to expand research across the state.
When UAMS needed remnant blood samples for the Arkansas
Coronavirus Antibodies Seroprevalence Survey last year, research leaders had the luxury of tapping a new resource for help: the UAMS Rural Research Network (RRN). Established in January 2020, the RRN increases researchers’
access to communities across Arkansas through our eight Regional Campuses, while helping to ensure Arkansas’ rural underrepresented
populations have access to community health resources and are included in health research.
The RRN was started with support from the Translational Research Institute (TRI); UAMS Office of the Provost, led by Stephanie Gardner, Ed.D., Pharm.D., also chief academic officer and chief strategist; the UAMS Office of Community Health & Research, led by Pearl McElfish, Ph.D., MBA; Regional Campuses, led by Amy Wenger, vice chancellor; and the Winthrop P. Rockefeller Cancer Institute, led by Michael J. Birrer, M.D., Ph.D., vice chancellor. Representatives of the Rural Research Network from across Arkansas meet via Zoom to discuss the COVID-19 seroprevalence survey.
This is an exciting intrainstitutional partnership because it presents new research and community engagement opportunities that are more inclusive of rural Arkansas. Having this network available is critical as we seek National Cancer Institute Designation.
Michael J. Birrer, M.D., Ph.D.,
By May 2021, the RRN was assisting nine studies, with an additional five studies pending.
The RRN delivered key support at a critical time in the statewide seroprevalence study, supplementing blood collections from volunteers and
UAMS clinics in Little Rock. The Family Medical Centers within the Regional Campuses at Fayetteville, Fort Smith and Pine Bluff contributed more than 1,300 remnant samples.
Working with the RRN team on the COVID-19 Seroprevalance study was both enjoyable and interesting. Our clinical lab was able to provide blood samples from NW Arkansas, and the regular research team meetings by Zoom were helpful in keeping participants engaged and up-to-date with regular progress reports. We would be glad to participate again when new projects come along.
Ronald Brimberry MD, UAMS Northwest
Affiliated Community Hospitals & Partners
We are grateful for the leadership and commitment of all our faculty, staff, institutional leaders and community partners who are central to the success of our programs. We hold formal affiliation agreements with the hospitals below as host institutions and training facilities. Deep appreciation is extended to these partners, which contribute facilities, funds, and staff to support our programs.
UAMS East
- Crittenden Memorial Hospital
- Helena Regional Medical Center
- Chicot Memorial Hospital
UAMS North Central
- White River Medical Center
- Baxter Regional Medical Center
- Woodlawn Heights Nursing Home
UAMS Northeast
- St. Bernards Regional Medical Center
- NEA Baptist Memorial Hospital
UAMS Northwest
- Washington Regional Medical Center
- Northwest Medical Center –Springdale
- Arkansas Veterans Home – Fayetteville
- Northwest Health Physicians’ Specialty Hospital
- Springdale Health and Rehabilitation Center
UAMS South
- Magnolia Regional Medical Center
- Arkansas Children’s Hospital – Little Rock
- Medical Center of South Arkansas – El Dorado
UAMS South Central
- Jefferson Regional
UAMS Southwest
- CHRISTUS St. Michael Health System
- Wadley Regional Medical Center
UAMS West
- Baptist Health Fort Smith
- Affiliated Community Hospitals & Partners
Key Partnership Highlights
Working with our partners at the Arkansas Rural Health
Partnership (ARHP), we successfully implemented an ACT-prep
program for high school students in southeast Delta counties, purchased a new mobile health unit (see below), and engaged 40 Delta students through internships at ARHP hospitals.
We successfully introduced new clinical rotations for eight 3rd and 4th year medical students to 10 federally qualified community health centers, working closely with our partners at the Community Health Centers of Arkansas (CHCA). Rotation schedules are now being
planned AY 2021- 2022.
Many new and exciting programs were launched this year in
partnership with our Historically Black Colleges and University
(HBCU) partners at the University of Arkansas at Pine Bluff and Philander Smith College.
We work closely with the UAMS Division of Diversity, Equity, and Inclusion (DDEI) to coordinate programs geared toward underrepresented minority students. This year, we collaborated with them and other UAMS colleges on a data recruitment module that will integrate with Regional Campuses’ database, significantly enhancing our institutional abilities related to tracking and communications with students.
Arkansas Farm Bureau is a long-term partner making possible our M*A*S*H* and CHAMPS summer camps across the state.
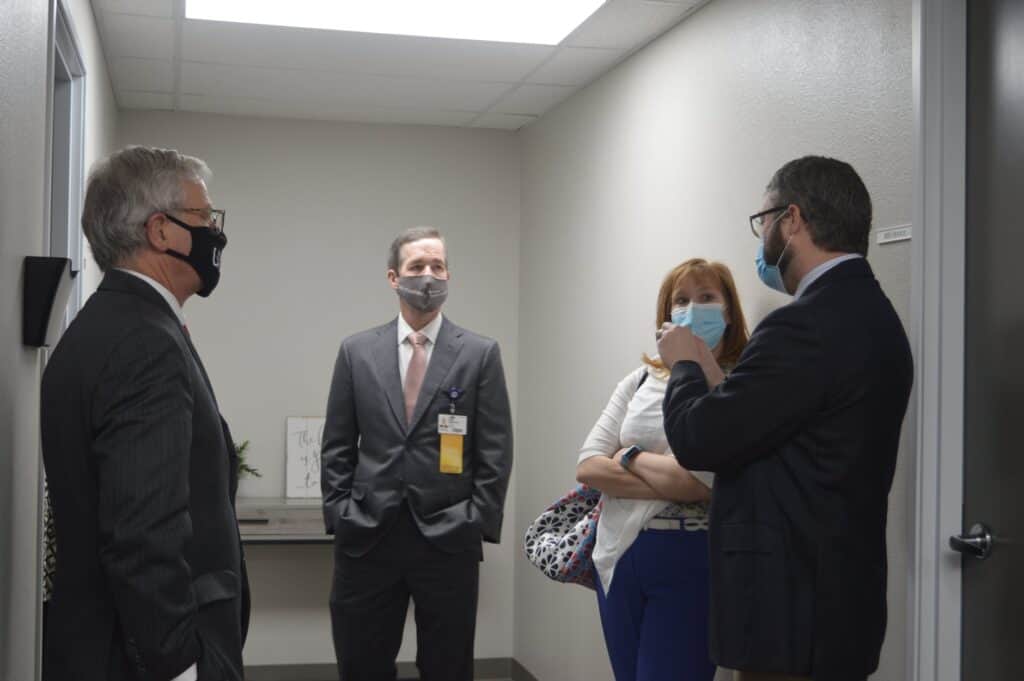
Hitting the Road!
This new mobile unit is hitting the streets of South Arkansas to provide students with an interactive experience to learn about various health careers on-site at schools, community events, and career and health fairs. This is a joint project with UAMS Regional Campuses, College of Medicine, Arkansas Rural Health Partnership, and Community Health Centers of Arkansas, funded through the HRSA Medical Student Education grant. Students will learn about health careers from fellow Arkansans who work in healthcare. Students will get to learn about the need for various providers, where they can be trained, how long it will take, and potential earnings. The mobile unit will serve communities statewide, and will also be available for other student and professional trainings and community outreach events.
The College of Medicine strives to ensure the highest quality of
Susan Smyth, M.D., Ph.D. Dean, College of Medicine Executive Vice Chancellor, UAMS
care for Arkansans and patients around the world. Improving access to high quality healthcare for rural and underserved Arkansans is a priority for UAMS and our college.